Abstract
Background: Hematopoietic cell transplantation (HCT) survivors have a complex and multiphase recovery period. Health care delivery and psychosocial interventions for HCT survivors are challenging as many HCT recipients live great distances from the facility where they had their HCT. Therefore, identifying factors associated with a patient's capability to self-manage symptoms is an important focus of survivorship research. A patient's self-efficacy may be important for the successful management of major stressors associated with treatments and recovery. Here, we aimed to evaluate the impact of perceived self-efficacy on distress, quality of life (QoL), depression, and fatigue, and identify the factors associated with lower self-efficacy.
Methods: This cross-sectional study analyzed baseline data from a randomized controlled internet based self-management intervention trial (INSPIRE, NCT01602211) in adult (age 18 and older) survivors 2-10 years post HCT. Patients with recurrence or subsequent malignancy requiring cancer treatment during the two years prior to enrollment, inability to read and understand English and lack of access to email and the Internet were excluded. Data included medical records and patient-reported outcomes (PROs) including Cancer and Treatment Distress (CTXD) with 6 subscales, Patient Health Questionnaire depression scale (PHQ-8), Short Form 12 Health Survey (SF-12) physical function (PCS) and mental function (MCS) scores, Brief Fatigue Inventory (BFI) and Health Self-Efficacy. Pearson correlations were used to test bivariate associations for self-efficacy with CTXD, SF-12, BFI, and PHQ8. General linear models were used to test the independent association for CTXD and SF-12 outcomes with self-efficacy, controlling for selected sociodemographic and treatment covariates. Tenability of statistical model assumptions were examined, and no remediation was necessary.
Results: Total of 1078 HCT survivors were included in the analysis. Participants were 18 to 76 years (mean age 51), 53% male, and over 90% white and non-Hispanic. Only 16% reported living in a rural area. A majority received an autologous HCT (55%) and were less than 5 years from their first HCT (54%). Among the allogeneic HCT recipients, more than half (60%) had active chronic Graft-versus-Host (cGVHD) and nearly 40% were on active systemic treatment. The mean self-efficacy score was 3.01 (SD 0.49). Female gender (p=0.014), younger age at HCT, younger age at cGVHD presentation, moderate to severe currently active cGVHD (p=0.003) and household income less than $40,000 (p < 0.001) were associated with lower self-efficacy. In bivariate analyses, self-efficacy was negatively correlated with mean total CTXD (r -0.5, p <0.001) and each of the CTXD subscales including family strain (r -0.41, p<0.0001), identity (r -0.37, p<0.0001), uncertainty (r -0.5, p<0.0001), interference (r -0.47, p<0.0001), medical (r -0.36, p<0.0001) and health burden (r -0.42, p<0.0001). HCT survivors with higher self-efficacy also reported better physical (r 0.48, p<0.001) and mental function on the SF-12 (r 0.57, p<0.001). Moreover, self-efficacy was negatively correlated with symptoms such as fatigue (r -0.44, p<0.001) and depression (r -0.48, p<0.001).
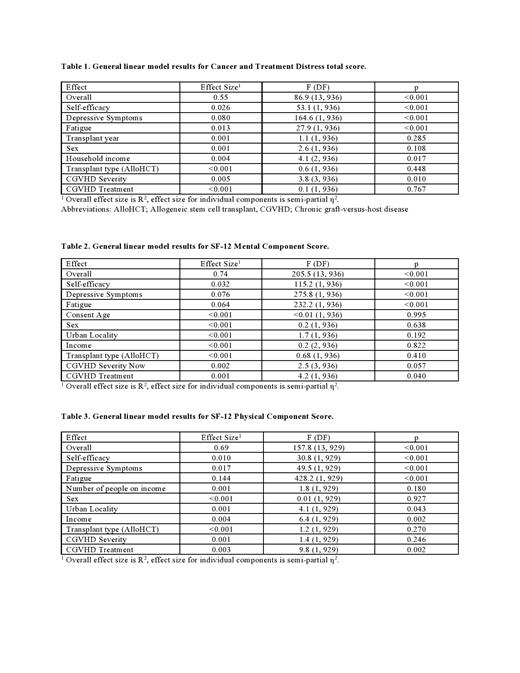
In a regression model investigating the impact of self-efficacy on CTXD controlled for demographics and disease characteristics , lower self-efficacy was independently associated with higher CTXD (beta -0.232; 95% CI (-0.294, -0.169), p< 0.001) (Table 1). Moreover, there was a significant positive relationship between self-efficacy and both mental (beta 4.68; 95% CI (3.82, 5.54); p <0.001) (Table 2) and physical (beta 2.69; 95% CI (1.74, 3.64); p<0.001) (Table 3) components of QoL.
Conclusion: Our study demonstrates that lower levels of self-efficacy reported by HCT survivors was independently associated with higher levels of symptoms such as fatigue and depression, lower QoL, and more cancer -related distress. Furthermore, self-efficacy is more likely to be impaired in females, younger adults, those with lower incomes, and survivors with active cGVHD. These findings support the value of self-management interventions focused on improving self-efficacy as having the potential to improve multiple symptoms and QoL in HCT survivors.
Farhadfar: Incyte: Consultancy. Jim: RedHill Biopharma: Consultancy; Janssen Scientific Affairs: Consultancy; Merck: Consultancy; Kite pharma: Research Funding. Majhail: Anthem, Inc: Consultancy; Incyte Corporation: Consultancy. Wingard: Merck: Consultancy; AlloVir: Consultancy; Celgene: Consultancy; Shire: Consultancy; Janssen: Consultancy; Cidara Therapeutics: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal